Title: Micro-Patching: A Revolutionary Approach to Burn Treatment
Introduction
Severe burn injuries present significant challenges in treatment and recovery, often requiring extensive skin grafting procedures that can be traumatic for patients. However, an innovative technique called micro-patching, which combines the precision of robotic surgery with the latest advancements in regenerative medicine and tissue engineering, offers a promising solution to revolutionize burn treatment.
The Micro-Patching Concept
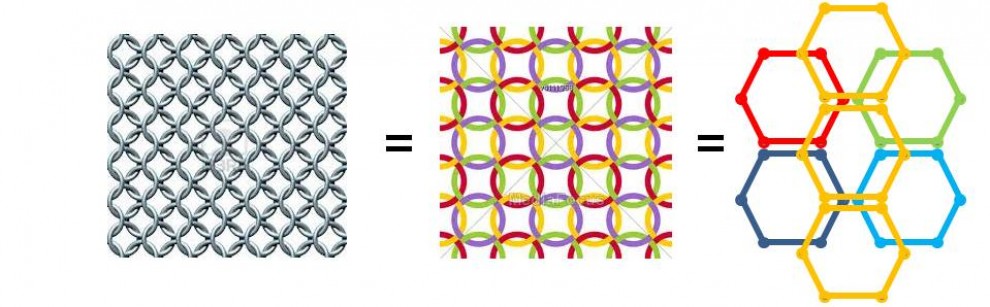
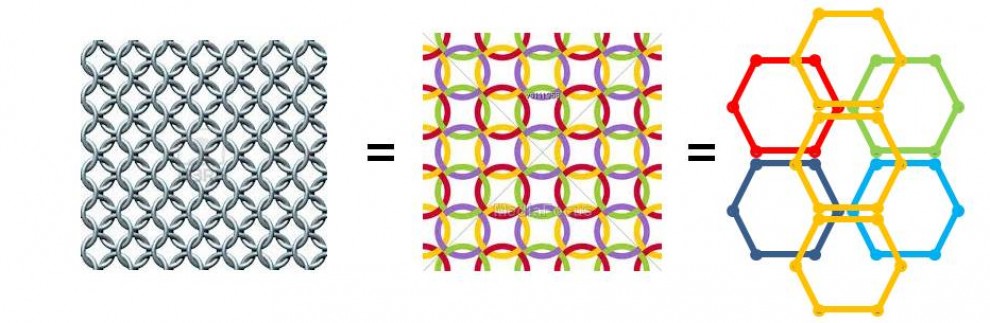
Micro-patching involves using a robotic surgical system to harvest tiny, checkerboard-patterned skin grafts from healthy donor sites on the patient’s body. These micro-grafts, comprising just 50% of the skin in the treated area, are then transplanted to the burn site, leaving the remaining 50% as empty spaces. The interspaces are then filled with a synthetic or bio-engineered matrix that supports and guides the regeneration of new skin tissue.
Advantages of Micro-Patching
- Minimally Invasive: By harvesting only half of the skin from the donor area, micro-patching minimizes the trauma and scarring associated with traditional skin grafting methods.
- Maximizing Donor Skin Utilization: The 50% micro-graft approach effectively doubles the area that can be treated with the same amount of donor skin, which is particularly valuable in cases of extensive burns where healthy skin is limited.
- Promoting Healing and Integration: The interlacing of micro-grafts with a supportive matrix promotes wound healing, reduces scarring, and facilitates the integration of the transplanted skin with the surrounding tissue.
Robotic Precision in Micro-Patching:
The integration of robotic systems in micro-patching is not just a technological marvel but a cornerstone of this innovative approach. These advanced robotic platforms offer unprecedented precision and consistency, significantly reducing the margin of error compared to traditional manual procedures. By employing laser-guided tools and AI-driven algorithms, the robots can harvest and transplant micro-grafts with meticulous accuracy, ensuring optimal placement and orientation. This level of precision is crucial for the checkerboard pattern of micro-grafts to seamlessly integrate with the synthetic matrix, facilitating a more natural and efficient healing process. The use of robotics also opens the door to less invasive surgeries, quicker recovery times, and minimized scarring, marking a significant step forward in patient care.
The Role of Nature in Skin Regeneration
While the human body has a remarkable capacity for skin regeneration, the process can be slow and may result in suboptimal outcomes, especially in the case of large or deep burns. If micro-patching were to be performed without the use of a supportive matrix, leaving the interspaces empty, the natural healing process would still occur. Epithelial cells would migrate into the empty spaces, proliferating and eventually covering the gaps. However, this natural regeneration is limited by factors such as wound size, the presence of a conducive environment for cell growth, and the availability of essential nutrients and oxygen.
Integrating a Matrix for In Situ Skin Growth
To overcome the limitations of natural healing and ensure more uniform and functional skin recovery, micro-patching incorporates a matrix that mimics the extracellular matrix of the skin. This scaffold provides a framework for cells to adhere to, grow, and eventually form new skin tissue. The ideal matrix should be biocompatible, promoting cell attachment and proliferation, and biodegradable, gradually dissolving as natural skin tissue replaces it. Materials such as hydrogels, which closely mimic the natural skin environment, and biodegradable polymers, designed to degrade at a rate matching skin tissue regeneration, are promising candidates for this application.
Innovations in Biodegradable Matrix Design: The development of biodegradable matrices for use in micro-patching represents a fusion of materials science and biomedical engineering. These matrices are designed to mimic the natural extracellular matrix of the skin, providing a scaffold that supports cell adhesion and growth. Engineered from polymers such as polylactic acid (PLA) and polyglycolic acid (PGA), or natural substances like collagen and alginate, these matrices gradually degrade at a controlled rate. This degradation is synchronized with the body’s own tissue regeneration process, ensuring that as new skin tissue forms, the scaffold dissolves, leaving no trace behind. This process not only supports the formation of healthy, new skin but also reduces the need for subsequent surgeries to remove non-biodegradable materials, enhancing the overall healing experience for patients.
Protective Measures and Healing Timeline
To prevent infection, maintain moisture levels, and protect the vulnerable new tissue from mechanical damage, the treated area should be covered with a protective case or shell. This semi-permeable covering allows for gas exchange, enabling the wound to ‘breathe’ while keeping it moist and protected.
The timeline for skin regeneration using a matrix depends on factors such as the extent of the burn, the patient’s overall health, and the specific materials and cell types used. Initial cell migration and proliferation could begin within days after the procedure, with the formation of a new epidermal layer over the matrix taking several weeks. Complete integration and maturation of the regenerated skin may extend over several months, during which the biodegradable matrix gradually dissolves, leaving behind newly formed skin tissue.
Enhancing Patient Experience Through Micro-Patching: Micro-patching stands out not just for its technological and biological innovations but for its patient-centric approach to burn treatment. By significantly reducing the need for large donor skin areas, this method lessens the physical and emotional burden on patients, making the healing journey less daunting. The minimized scarring and faster recovery times associated with micro-patching can have profound effects on a patient’s self-esteem and mental health, often critical aspects of recovery that are overlooked in traditional treatments. Furthermore, the less invasive nature of the procedure, combined with the potential for reduced pain and discomfort, underscores the commitment of micro-patching to not only heal the body but also to nurture the patient’s overall well-being.
Enhancing Micro-Patching with Advances in Regenerative Medicine
The potential of micro-patching can be further enhanced by incorporating cutting-edge developments in regenerative medicine:
- Lab-Grown Skin Cells: Integrating lab-grown skin cells, such as keratinocytes and fibroblasts, derived from the patient’s own tissue into the synthetic or bio-engineered matrix could improve healing and reduce the risk of rejection.
- Stem Cell Integration: Incorporating stem cells into the matrix has shown promise in promoting more versatile and resilient skin tissue regeneration.
- Advanced Biomaterials: Researchers are exploring various biomaterials, such as hydrogels and biodegradable polymers, to create skin substitutes that closely mimic the natural skin environment and promote better integration with the patient’s tissue.
Challenges and Future Directions
While micro-patching holds immense potential, several challenges need to be addressed:
- Technological Advancements: Further development of precise robotic systems and refined techniques for harvesting and transplanting micro-grafts will be crucial.
- Clinical Trials and Safety: Extensive research, including clinical trials, will be necessary to demonstrate the safety, feasibility, and effectiveness of micro-patching.
- Regulatory and Ethical Considerations: Micro-patching will need to navigate regulatory approvals and address ethical concerns related to patient access and informed consent.
- Surgeon Training: Implementing micro-patching will require specialized training for surgeons and medical staff to effectively use the robotic systems and manage the integration of micro-grafts and synthetic matrices.
Conclusion
Micro-patching represents a transformative approach to burn treatment, leveraging the synergy between robotic precision, regenerative medicine, and the body’s natural healing processes. By minimizing trauma, maximizing donor skin utilization, and promoting efficient healing through the integration of micro-grafts and supportive matrices, micro-patching has the potential to revolutionize burn care.
As research and development in this field continue, micro-patching could offer new hope for burn patients, improving outcomes, reducing scarring, and enhancing quality of life. While challenges remain, the promise of this innovative approach is significant, and its successful implementation could mark a major milestone in the advancement of burn treatment and patient care. As advancements in materials science, stem cell research, and tissue engineering converge with the micro-patching technique, we can anticipate even more sophisticated and personalized solutions for skin regeneration in the future.