The web has enabled transformation of most industries to some degree. In effect, the whole range of mechanisms for provision of services of all kinds has been decomposed and rebuilt. However, it will take many years for all these potential changes to become in-reality and then to ripple through all organisations.
This is true in all industries, so we see an interesting dynamic where new companies enter a market using new technology and new techniques to compete head on with existing traditional institutions. These often rely on their corporate and political power, influence and sheer momentum for their survival while they start to adapt to changes that they realise will prove irresistible even for them. But they must adapt, or eventually die.
Healthcare is no exception. Resources are limited, while demand is accelerating due to increasing expectations driven by everyday experience in other areas of life. People expect to live longer and to be healthier. They expect drugs, technologies, and medical knowledge and expertise to progress continuously, and to be given access to it. If and where it doesn’t, people perceive it as a fault.
We are now approaching the limits of sustainability of such expectations. State resources can’t be increased significantly beyond overall economic growth and are of course likely to actually reduce in the short to medium term. The only mechanisms left to improve health care now are to make it more efficient, to do more with less via better technology, organisation structures, or to use other groups to increase the resources available beyond state funding.
Once we start to look beyond the state, we see much greater resource availability, of which individual desire to be healthy takes pole position, with the desire to also be financially secure also taking a strong place. Many people already spend heavily on sports for example, and they can make a valuable contribution to a healthy life. This links well to many other forms of self help, such as eating better food, do-it-yourself health care via web information, using self help groups for advice instead of doctors and so on. All these are natural derivatives of social web advances.
If people start to perceive a gap between what they want and what the state provides, then such groups are likely to fill it.
Life insurance pays out when people die, but the later that is, the longer they are able to receive interest on the money paid in. It is in the interests of life insurers also to underestimate longevity, since the charges they can levy depend on the perceived risk of dying in a particular year, which they overstate, so their charges may well be higher than they need to be. This presents an opportunity to cultivate a trust-based relationship in place of the standard adversarial one, beating them in brand loyalty, by giving more accurate information to customers where they are more used to being manipulated by skilful marketing. Pension providers perversely have an incentive to reduce life span for retired people, so can’t be expected to help with schemes to improve health for the elderly, but they do have a positive incentive to keep people in good health while they are working, and hence paying into schemes. If people die early, i.e long before they retire, then pensions often have to pay lump sums in excess of payments received, so it is this part of pensions industry that may be useful in addressing health care. So it is clear that the finance industry sometimes but not always has the best interests of the customer at heart, i.e. when they are aligned with their own.
Insurance gives an additional incentive for people to improve the care they take of their own health. Health insurance is already sometimes linked to membership of health clubs, but could also take account of supermarket purchases for a family. If however, social media were to continue to develop along the lines of the current online buying communities, then large social groups could start self-insuring themselves, removing the profit element and reducing cost, without the big brother aspects of policing via insurance company. Of course, if these groups make sure that they comprise members mainly with good attitudes to looking after their own health, then their costs would be lower than the population as a whole. This self-organising local finance has much in common with the roots of the old building society model, and assisted by people’s familiarity with the web, it may well come back in direct competition with established banks and finance companies.
There is also a natural synergy here with social network sites linking in to sports clubs. Engaging in sports generally improves health, but it also provides opportunities for social networking, and if these are made better using improving technology, more people may do more sports and keep fitter. Linking to self insurance communities, large groups of people could do what they can to keep in good health, reducing their health costs. Similarly, adding immersive gaming and entertainment can make sports such as running or cycling or other gym activity more fun at potentially little extra cost.
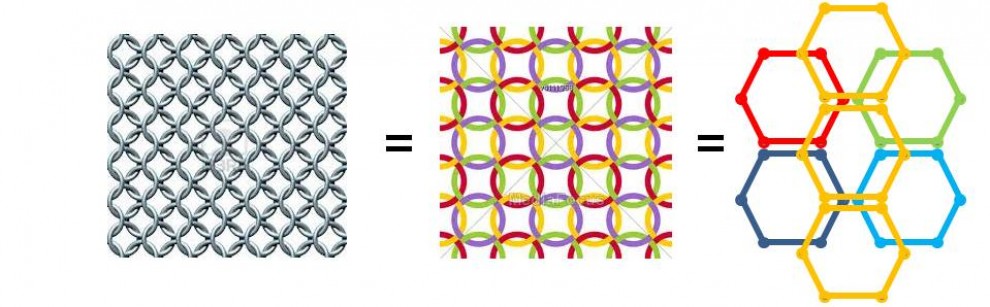
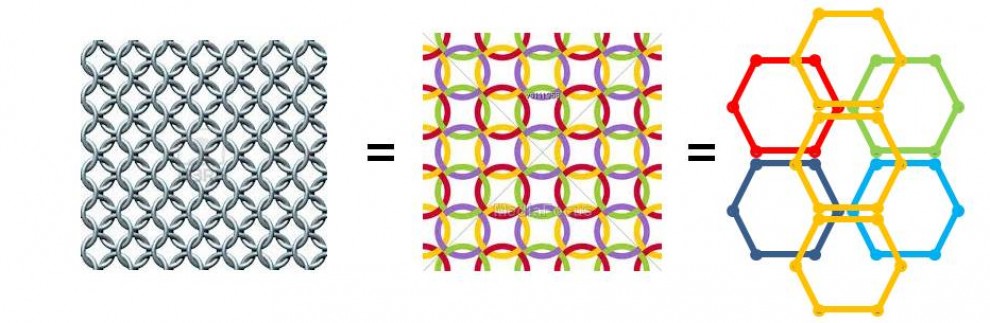
Artificial intelligence will play a big part in future health care too. Already expert systems play a key role in diagnosis, and many GPs can’t do as well on their own as an expert system. So today we have nurses on NHS Direct enabled to execute early stages of diagnosis and deciding with the computer whether a real GP is needed or not. In the future, as they get more used to AI, people may directly use online AIs without any perceived need to talk to a nurse or GP at all unless they need to get a prescription or treatment. Even that looks like to be increasingly outsourced to pharmacists, who could of course easily be copied in on any diagnostic process, and make up their own minds about the personal integrity and state of the patient needing the prescription. This could save a great deal of health costs. In fact, we may perceive various rings of care, with hospitals and clinics in the centre with expert staff, surrounded by technicians using AI, and then a large ring of self help groups, social networks, sports clubs and insurance companies all offering assistance, and of course many people will be able to find their problems via self diagnosis anyway, and frequent self treatment.
This will be highly incentivised by rationing of state provision. Regardless of party intentions, medical technology will become more and more powerful and demand will rise insatiably. People have to accept that they can only have some medical care provided by the state.
Social networks naturally care for people in their midst to some degree. Humans are tribal by nature. The degree to which on-line social networks fit this same anthropology is debated, but some social networks also relate to local geography, and these add a means of strengthening local community, enhancing bonds. As the social web continues to improve, and as positioning systems make the links to the physical world more tangible, so we should expect crystallisation of social networks into community networks too. These will provide an excellent platform for care in the community, ensuring that old and frail people can find local support, but only provided that the local society actually has the willingness available. Such networks can liberate the latent caring and willingness of communities, but cannot be expected to create it. Social health is quite a different matter from the technology support platform.
Similarly, home care can be helped enormously by having good networks, especially when coupled with webcams. People can video link with health workers or other people, reducing loneliness and providing care without the need to travel. This could make it much easier to provide independence and continuation of dignity as people age. Tomorrow’s older people will have aged in the background of technology availability and it will not so much possible as expected for them to access care and support using the network. They will not question being ‘fobbed off’ with cheaper net based solutions, but rather will treat them as the proper mechanism, and more likely resent it when they have to travel to access care when they know it could have been done more simply, cheaply and with less hassle across the net. Government and health providers should capitalise on this as far as possible to reduce costs. Insurers also may have some ability to force the use of such solutions, by only providing funding for the most cost effective care mechanism.
With all the economic pressures caused by rising health costs, increasing longevity and rising expectations of comfort, there is one major pressure on the system that is an internal social stress. Inter-generational conflict is highly likely to result if a younger generation sees that they are having to fund large gaps in the costs of an older generation compared to what they paid into the system,. With government forced to make cuts all over the economy, pressure groups are strongly resisting any reduction in the benefits already due to an ageing population that are actually far in excess of their payments into the system. Having voted for unaffordable benefits over the last decades, increasing longevity has greatly increased the value of them still further, especially pensions, but also health care costs. If government continues to defend such benefits to existing beneficiaries from erosion, and instead blocks future generations from receiving them, although they still have to fund them, this can only end in trouble. We should expect strong resistance from young people to funding costly benefits to which they are not themselves entitled. As yet, this realisation of the discrepancy between the benefits and costs accrued by different generations has not materialised. Indeed, the current demonstrations in France against pension age increase show surprising ignorance by the younger population, who appear to imagine that they will be spared from harsh reality themselves even though their retirements are many years away. All the demonstrators want future generations to pick up the bills, and of course that is also blatantly true here in the UK. But democracy is fragile, and requires that all sections of the population believe they are treated reasonably fairly. Ignorance of the degree to which younger people are currently being abused will not last, and the one-sided policies that substantially favour older people over younger people will not survive for long.
The nightmare scenario for inter-generational conflict is that if taxes rise too far to pay the deficit between payment in and benefits out for older people, then younger people who have good career options overseas may well take them, and as they leave, so do their taxes. It is not inconceivable that we could end up with a retirement home UK, with lots of expensive older people, and the less talented, and hence poorer, younger population, with a brain drain taking many of the best of the population elsewhere to less exploitative areas. That of course would be even less sustainable, all the more reason to prevent such a situation ever arising in the first place.
So there are many options for reducing the costs of health care, and in the background, other increasing pressures to do so. Health insurance companies have many options to work imaginatively with a well networked society for mutual benefit, and if they don’t bother to do so, then society will likely do so for itself via social entrepreneurs.





I take your point that Healthcare as it is now is unsustainable as a public institution, and that it should be supplanted by various other privately owned institutions; but what about me? As a 17 year old who has just recovered from Leukemia and has on-going medical issues, how would I get insurance? No company in their right mind would take me, due to my large medical bills, or if they did, they would charge me so much that it would be ridiculous. What kind of plan would there be in place, if any, for people like me, who have expensive medical conditions that would make it very difficult for them to get insurance? How would I afford to go to medical school if I have to pay excessive medical insurance bills?
LikeLike
Good point, but the countries that use insurance based schemes also have provision for such cases as yours, where the state pays. Certainly if swapping over from NHS style coverage to insurance-based, the UK would have to legislate cover for all existing conditions, and make sure companies offer cover even to people with high risks.
LikeLike