1. Introduction
The human gut microbiome, consisting of trillions of microorganisms, plays a crucial role in maintaining overall health and well-being. Imbalances in the gut microbiome, known as dysbiosis, have been linked to a wide range of diseases, including metabolic disorders, autoimmune conditions, and even mental health issues. Current approaches to managing the gut microbiome, such as probiotics and dietary interventions, have shown limited success in addressing these complex health challenges.
Recent advances in synthetic biology and artificial intelligence (AI) have opened up new possibilities for targeted, personalized interventions in gut health. The concept of a Synthetic Biome Manager (SBM) and Parallel Immune System (PIS) represents a novel approach to monitoring, modulating, and optimizing the gut microbiome, with the potential to revolutionize the prevention and treatment of gut-related diseases.
This paper explores the concept of the SBM and PIS, their key components and functionalities, and the challenges and opportunities associated with their implementation. We also discuss the potential synergy between these systems and the Enhanced DNA (EDNA) framework, highlighting the transformative potential of these technologies for personalized medicine and public health.
2. The Synthetic Biome Manager (SBM)
2.1. Overview of the SBM concept
The Synthetic Biome Manager (SBM) is a proposed system of AI-driven, synthetic biological entities designed to monitor and modulate the gut microbiome in real-time. The SBM would consist of a network of sensors, actuators, and intelligent control systems that work together to maintain a healthy and balanced gut ecosystem.
2.2. Key components and functionalities
The SBM would include the following key components:
– Biosensors: Miniaturized, biocompatible sensors that can detect specific microbial species, metabolites, and other biomarkers in the gut environment.
– Actuators: Synthetic biological entities capable of releasing targeted antimicrobial agents, prebiotics, or other modulatory compounds in response to specific triggers or AI-generated instructions.
– AI control system: A centralized, AI-driven control system that integrates data from the biosensors, analyzes patterns and trends, and generates personalized interventions to optimize gut health.
2.3. AI-driven monitoring and modulation of the gut microbiome
The AI control system would continuously monitor the gut microbiome, identifying imbalances, pathogenic strains, and potential threats to gut health. By analyzing vast amounts of data from the biosensors and comparing it with reference datasets of healthy gut microbiomes, the AI system would generate targeted interventions to restore balance, impeding and culling harmful populations and promoting the growth of beneficial microbes.
These interventions could include the release of specific antimicrobial agents to eliminate harmful bacteria, the delivery of prebiotic compounds to support the growth of beneficial strains, or the modulation of the gut environment to create conditions that favor the establishment of a healthy microbiome.
The SBM’s AI control system would not only monitor an individual’s gut microbiome but also contribute to a collective, hive-like AI knowledge base of what constitutes a healthy gut microbiome across a diverse population. By analyzing data from numerous SBMs in healthy individuals, the AI system can identify a broad range of acceptable ‘styles’ or configurations of the gut microbiome that are associated with optimal health outcomes. This knowledge base would allow individual SBMs to make informed decisions about the necessary interventions to maintain or restore a healthy gut microbiome, while avoiding unnecessary changes to a well-functioning microbiome that may have a different but equally acceptable composition.
2.4. Personalized gut health optimization
One of the key advantages of the SBM is its ability to provide personalized, adaptive interventions based on an individual’s unique gut microbiome profile. The AI control system would learn from the specific responses of an individual’s gut microbiome to various interventions, continuously refining its strategies to optimize gut health.
This personalized approach could potentially enable the development of precision therapies for a wide range of gut-related diseases, taking into account individual variations in genetics, diet, lifestyle, and environmental factors. Within the basket of healthy styles, some will be more helpful in supporting recovery from particular diseases or preventing their worsening. Knowledge of what works and doesn’t work for disease groups will accumulate as AIs continuously share their data. For example, large numbers of people suffer from diabetes or ulcers. Knowing the best biomes to avoid these from ever taking hold, and recognizing signs that there is a risk of them, will be extremely useful, as of course would be the nature of the best restorative biome.
Clearly, the optimum biome may not stay the same for any person, but adapt and change according to detected health risks, or indeed actual diseases present.
It is also important that changes intended to address one disorder do not increase the risk of another one. It is possible under some circumstances that a temporary change to solve a problem might incur a risk cost or actual illness temporarily, much like chemotherapy incurs a short term suffering to fix a serious illness.
2.5. Continuous monitoring and adaptive intervention
To effectively maintain a healthy gut microbiome, the SBM must continuously monitor the dynamic changes in the gut environment, which can be influenced by various factors such as diet, medication, and stress. Microfluidic analysis technology, or adaptations thereof, could be integrated into the SBM to enable real-time, high-resolution profiling of the gut microbiome and its metabolic activities.
By analyzing this continuous stream of data, the SBM’s AI control system can identify subtle shifts in the gut microbiome composition and function, allowing for early detection of potential imbalances or dysbiosis. However, it is crucial that the SBM distinguishes between normal, transient fluctuations in the gut microbiome and persistent deviations that warrant intervention.
The hive-like AI knowledge base, built from data collected across a diverse population, would provide the necessary context for the SBM to make these distinctions. By comparing an individual’s gut microbiome profile to the range of acceptable configurations identified in the knowledge base, the SBM can determine whether an intervention is needed and, if so, what specific actions should be taken to restore balance.
This adaptive, context-aware approach to gut microbiome management ensures that interventions are targeted, timely, and minimally disruptive to the overall gut ecosystem. By leveraging the power of continuous monitoring and hive working, the SBM can provide a personalized, dynamic, and responsive solution for maintaining optimal gut health.
2.6. Considerations for integrating additional IT/biotech devices
While the Synthetic Biome Manager (SBM) and Parallel Immune System (PIS) offer a comprehensive, metabiological approach to monitoring and modulating the gut microbiome, it is worth considering the potential benefits and drawbacks of integrating additional IT/biotech devices to complement their capabilities.
Pros:
1. Comprehensive, spatially resolved gut mapping: An implanted electronic device equipped with an array of sensors could potentially provide a more detailed, real-time map of various parameters along the entire length of the digestive tract, such as pH, temperature, oxygen levels, and metabolite concentrations. This information could help identify localized abnormalities or areas of concern that may not be apparent from analyzing bulk samples.
2. Assessment of gut physical properties: An implanted electronic device could provide additional data on the gut’s physical properties, such as motility, contractility, and transit time. This information could be valuable in assessing the overall health and function of the digestive system and could help identify potential issues, such as intestinal blockages or dysmotility, that may not be directly related to the gut microbiome but could still impact gut health.
Cons:
1. Invasiveness and biocompatibility: Implanting electronic devices in the gut would require surgical procedures, which could introduce additional risks and complications. Ensuring the long-term biocompatibility and stability of these devices in the harsh gut environment would also be a significant challenge.
2. Power supply and data transmission: Implanted electronic devices would require a reliable power source and a means of transmitting data to external systems for analysis. Addressing these challenges could add complexity to the overall system and may require additional components or surgical interventions.
3. Limited duration and snapshot data: A swallowed electronic device for annual check-ups would only provide a snapshot of the gut health at a particular time point and may not capture the dynamic changes and interactions that occur over longer periods. The limited duration of monitoring and the inability to provide real-time, continuous data could reduce the overall value of such a device.
4. Potential redundancy: The SBM and PIS, as proposed, already offer a comprehensive and adaptable solution for maintaining gut health through AI-driven monitoring, hive working, and targeted interventions. The introduction of additional electronic devices may not provide significant benefits over the existing metabiological approach in many cases.
Conclusion:
While implanted electronic devices could potentially offer some additional capabilities, such as comprehensive, spatially resolved gut mapping and assessment of gut physical properties, the SBM and PIS, as metabiological systems, already provide a powerful and flexible approach to maintaining gut health. The potential benefits of integrating additional IT/biotech devices should be carefully weighed against the invasiveness, biocompatibility concerns, and potential redundancy with the existing metabiological solution. As research in this area advances, it may be valuable to explore the potential synergies between metabiological systems and electronic devices to identify specific use cases where a combination of these approaches could provide additional benefits. However, for the majority of applications, the SBM and PIS, as proposed, offer a comprehensive, adaptable, and minimally invasive solution for maintaining gut health.”
3. The Parallel Immune System (PIS)
3.1. Overview of the PIS concept
The Parallel Immune System (PIS) is a proposed companion system to the SBM, designed to work in tandem with the body’s natural immune system to provide enhanced protection against pathogens and harmful microbes in the gut. The PIS would consist of a network of synthetic immune cells and signaling molecules that can detect and respond to threats in the gut environment.
Synthetic immune cells could be designed by AI and a lab-grown culture introduced into the patient either by suppository or via a syringe.
Discuss a TNCO alternative to using cells. A TNCO has no particular form but could grow among and even around other organisms. It could reduce to minimal size and ‘hibernate’ in tiny crevices in gut walls until the AI instructs its growth to address some problem.
A TNCO would also be AI designed and lab-made, but a large number of TNCO variants/species could by introduced in a single injection or suppository. Hundreds could fit in a single drop.
3.2. Integration with the SBM
The PIS would be fully integrated with the SBM, sharing data and coordinating responses to optimize gut health. The biosensors and AI control system of the SBM would provide real-time information about the presence of pathogens or other threats, allowing the PIS to mount targeted, rapid responses.
3.3. Enhancing the body’s natural defense mechanisms
The synthetic immune cells of the PIS would be designed to mimic and enhance the functions of natural immune cells, such as macrophages, dendritic cells, and T cells. These synthetic cells would be equipped with advanced pattern recognition receptors and signaling pathways that enable them to detect and respond to a wider range of threats than the natural immune system.
In addition, the PIS would include synthetic signaling molecules that can modulate the activity of the natural immune system, boosting its response to specific threats or dampening excessive inflammation when necessary.
3.4. Targeted elimination of pathogens and harmful microbes
One of the key functions of the PIS would be the targeted elimination of pathogens and harmful microbes in the gut. Upon detection of a threat, the synthetic immune cells would release antimicrobial agents or engage in direct cell-to-cell contact to neutralize the pathogen.
The AI control system of the SBM would guide the response of the PIS, ensuring that the elimination of harmful microbes is targeted and precise, minimizing collateral damage to beneficial gut bacteria.
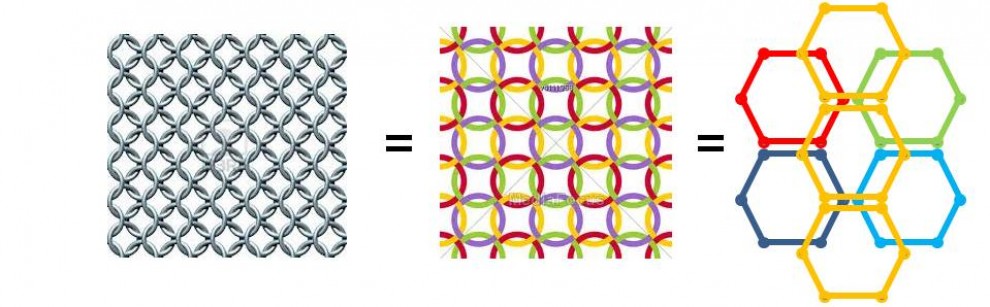
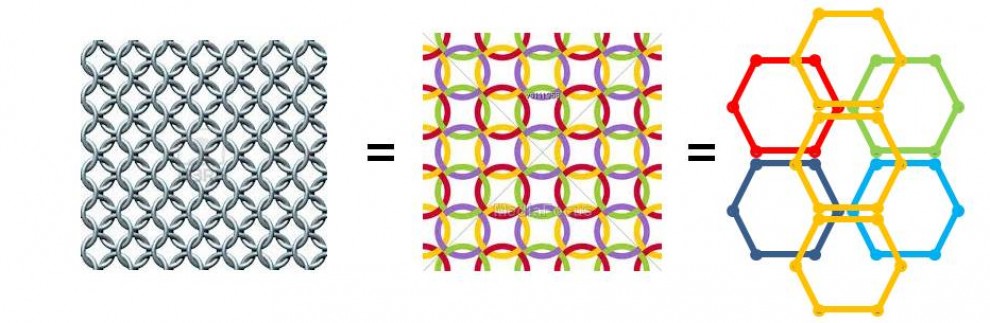
3.5. TNCO-based Parallel Immune System While the PIS can be implemented using synthetic immune cells, an alternative approach utilizing Tethered Non-Cellular Organisms (TNCOs) offers unique advantages. TNCOs are AI-designed, lab-made entities that do not have a fixed cellular structure, allowing them to adapt their form and function to the specific needs of the gut environment.
One of the key benefits of TNCOs is their ability to grow among and even around other organisms in the gut, enabling them to interact with and modulate the gut microbiome in ways that may not be possible with cellular agents. This adaptability could allow TNCOs to target specific pathogens or toxins, form protective barriers around beneficial microbes, or even facilitate the transfer of genetic material or metabolites between different species in the gut.
Another advantage of TNCOs is their ability to reduce to a minimal size and enter a state of hibernation, allowing them to persist in tiny crevices in the gut walls until they are needed. This hibernation capability enables the PIS to maintain a reserve of TNCOs that can be quickly activated by the AI control system in response to detected threats or imbalances in the gut microbiome.
The AI-driven design and production of TNCOs also allow for the creation of a diverse array of TNCO variants or species, each with unique properties and functions. This diversity can be leveraged to create a highly adaptable and resilient PIS, capable of responding to a wide range of challenges in the gut environment. Moreover, the small size of TNCOs means that hundreds of different variants could be introduced into the gut with a single injection or suppository, providing a highly concentrated and potent therapeutic payload.
The use of TNCOs in the PIS represents a novel and exciting approach to enhancing the body’s natural defense mechanisms and maintaining a healthy gut microbiome. By leveraging the unique properties of these non-cellular entities, the TNCO-based PIS could offer a more flexible, adaptable, and effective alternative to cell-based systems, opening up new possibilities for targeted, personalized interventions in gut health.
4. Implementation Challenges and Potential Solutions
4.1. Biocompatibility and safety
Ensuring the biocompatibility and safety of the SBM and PIS is a critical challenge. The synthetic biological entities and materials used in these systems must be designed to minimize the risk of adverse immune reactions, toxicity, or other unintended consequences.
Rigorous testing and validation of the biocompatibility and safety of these systems will be essential before they can be deployed in human subjects.
4.2. Long-term stability and adaptability
Another key challenge is ensuring the long-term stability and adaptability of the SBM and PIS in the dynamic environment of the gut. The synthetic biological entities must be able to survive and function in the presence of digestive enzymes, pH variations, and other stressors.
Moreover, the AI control system must be able to adapt to changes in the gut microbiome over time, learning from the specific responses of an individual’s gut to various interventions and adjusting its strategies accordingly.
4.3. Ethical and regulatory considerations
The development and deployment of the SBM and PIS will raise important ethical and regulatory questions. The use of synthetic biological entities and AI-driven interventions in the human body will require careful oversight and governance to ensure that these technologies are used safely and responsibly.
Engaging with bioethicists, regulators, and other stakeholders early in the development process will be essential to address these concerns and build public trust in these technologies.
4.4. Public acceptance and patient education
Achieving widespread public acceptance and adoption of the SBM and PIS will require a concerted effort to educate patients and the general public about the potential benefits and risks of these technologies.
Clear communication about the science behind these systems, their intended uses, and the safeguards in place to protect patient safety will be critical to building trust and support for their use in personalized medicine.
5. Development Timeline and Integration with EDNA
5.1. Near-term goals and milestones
The development of the SBM and PIS will require a phased approach, with near-term goals focused on proof-of-concept studies and early clinical trials. Key milestones in the near-term include:
– Demonstrating the feasibility and safety of the SBM and PIS in animal models
– Developing and validating the AI control system and its ability to generate personalized interventions
– Conducting first-in-human clinical trials to assess the safety and efficacy of these systems in small cohorts of patients with specific gut-related diseases
5.2. Long-term vision and potential applications
In the long-term, the SBM and PIS could be integrated into a comprehensive, personalized approach to gut health and disease prevention. These systems could be used to:
– Develop precision therapies for a wide range of gut-related diseases, including inflammatory bowel disease, irritable bowel syndrome, and colorectal cancer
– Optimize gut health in healthy individuals, promoting overall well-being and reducing the risk of developing chronic diseases
– Monitor and respond to changes in the gut microbiome throughout an individual’s lifespan, adapting to different life stages and health challenges
5.3. Evolution of the SBM and PIS with EDNA
As the SBM and PIS mature, their integration with the Enhanced DNA (EDNA) framework could lead to the development of a full body management system. EDNA’s advanced capabilities for monitoring and modulating biological processes at the cellular level could enable the extension of the SBM and PIS beyond the gut, creating a comprehensive, whole-body approach to health optimization.
This evolution could involve:
– Expanding the network of biosensors and actuators to other organ systems and tissues, allowing for real-time monitoring and modulation of various physiological processes
– Integrating data from multiple sources, including the gut microbiome, immune system, and other organ-specific biomarkers, to create a holistic view of an individual’s health status
– Developing more sophisticated AI algorithms that can analyze and interpret this complex, multi-dimensional data, generating personalized interventions that target multiple aspects of health simultaneously
– Incorporating advanced technologies, such as nanotechnology and tissue engineering, to enable more precise and targeted delivery of therapeutic agents and regenerative therapies
By leveraging the power of EDNA, the SBM and PIS could evolve into a transformative platform for whole-body health optimization, enabling a new era of personalized, predictive, and preventive medicine.
5.4. Synergy with other advanced technologies
In addition to EDNA, the SBM and PIS could be combined with other advanced technologies to create powerful platforms for personalized medicine and drug discovery. For example:
– Nanotechnology could enable the development of more sophisticated biosensors and actuators, allowing for even more precise monitoring and modulation of biological processes at the molecular level
– Organ-on-a-chip systems could provide a powerful tool for testing and validating the safety and efficacy of personalized interventions generated by the SBM and PIS, accelerating the translation of these technologies into clinical practice
– Advanced imaging techniques, such as super-resolution microscopy and functional magnetic resonance imaging (fMRI), could provide additional insights into the complex interactions between the gut microbiome, immune system, and other physiological processes, informing the design and optimization of the SBM and PIS
By harnessing the synergies between these advanced technologies, the SBM and PIS could become part of a larger ecosystem of personalized medicine tools, driving innovation and progress in the field of health optimization.
6. Conclusion
6.1. The transformative potential of the SBM and PIS
The development of the Synthetic Biome Manager and Parallel Immune System represents a potentially transformative approach to gut health and disease prevention. By leveraging the power of synthetic biology and AI, these systems could enable personalized, targeted interventions that optimize the gut microbiome and enhance the body’s natural defense mechanisms.
As the SBM and PIS evolve and integrate with EDNA and other advanced technologies, their potential impact could extend far beyond the gut, enabling a whole-body approach to health optimization that could revolutionize the field of personalized medicine.
6.2. Future directions and research priorities
To realize the full potential of the SBM and PIS, future research should focus on:
– Advancing our understanding of the complex interactions between the gut microbiome, immune system, and host genetics
– Developing more sophisticated AI algorithms for analyzing and interpreting the vast amounts of data generated by these systems
– Exploring the potential synergies between the SBM, PIS, EDNA, and other advanced technologies, such as nanotechnology and organ-on-a-chip systems
– Addressing the ethical, legal, and social implications of these technologies, ensuring their responsible development and deployment
6.3. Implications for personalized medicine and public health
The successful development and deployment of the SBM and PIS, and their eventual integration with EDNA and other advanced technologies, could have profound implications for personalized medicine and public health. These technologies could enable a shift towards a more proactive, preventive approach to healthcare, where individuals are empowered to optimize their health and reduce their risk of developing chronic diseases.
Moreover, by providing a powerful platform for precision therapies and drug discovery, the SBM and PIS could accelerate the development of new treatments for a wide range of diseases, improving outcomes and quality of life for millions of patients worldwide.
In conclusion, the Synthetic Biome Manager and Parallel Immune System represent an exciting and promising frontier in the field of personalized medicine and health optimization. As these technologies evolve and integrate with EDNA and other advanced tools, they could drive a transformative shift in how we approach health and disease, enabling a future where personalized, predictive, and preventive medicine becomes the norm.
7. Gut microbiome-related diseases and the potential impact of SBM/PIS
7.1. Introduction
The gut microbiome has been increasingly recognized as a critical factor in the development and progression of various diseases, ranging from gastrointestinal disorders to neurological conditions. Numerous studies have shown that alterations in the gut microbiome, known as dysbiosis, are associated with a wide array of health issues, including inflammatory bowel disease (IBD), irritable bowel syndrome (IBS), colorectal cancer, obesity, type 2 diabetes, autoimmune diseases, and even neurological disorders such as Parkinson’s and Alzheimer’s disease. Additionally, factors such as diet, genetics, and epigenetics have been found to interact with the gut microbiome, further influencing disease risk and progression.
The Synthetic Biome Manager (SBM) and Parallel Immune System (PIS) offer a promising approach to addressing gut microbiome-related diseases by continuously monitoring the gut microbiome, identifying dysbiosis patterns, and developing personalized interventions to restore balance and promote health. While the extent to which the SBM/PIS can provide a “cure” or long-term management solution may vary depending on the specific disease and individual factors, this innovative system has the potential to significantly improve patient outcomes and quality of life. In the following sections, we will explore the known links between various diseases and the gut microbiome, as well as the potential impact of the SBM/PIS on their prevention, management, and treatment.
7.2. Inflammatory Bowel Disease (IBD)
7.2.1. Known links to gut microbiome, diet, and genetic/epigenetic profile
Inflammatory Bowel Disease, which includes Crohn’s disease and ulcerative colitis, has been strongly linked to dysbiosis in the gut microbiome. Studies have shown that IBD patients often have reduced microbial diversity, with a decrease in beneficial bacteria such as Firmicutes and Bacteroidetes and an increase in potentially harmful bacteria such as Proteobacteria. Dietary factors, such as a high-fat, low-fiber Western diet, have also been associated with an increased risk of IBD. Genetic susceptibility plays a role in IBD, with several identified risk alleles involved in immune regulation, barrier function, and microbial recognition.
7.2.2. Potential impact of SBM/PIS on IBD management and treatment
The SBM/PIS could have a significant impact on the management and treatment of IBD by continuously monitoring the gut microbiome and identifying dysbiosis patterns associated with disease activity. The AI-driven system could then develop personalized interventions to restore balance in the gut microbiome, such as targeted probiotic therapy, dietary modifications, or the use of synthetic immune cells or TNCOs to modulate the immune response. By maintaining a healthy gut microbiome and preventing dysbiosis, the SBM/PIS could potentially reduce the frequency and severity of IBD flare-ups, improve quality of life, and possibly even induce long-term remission in some patients. However, given the complex nature of IBD and the involvement of genetic and environmental factors, a complete “cure” may not be achievable through microbiome modulation alone.
7.3. Irritable Bowel Syndrome (IBS)
7.3.1. Known links to gut microbiome, diet, and genetic/epigenetic profile
Irritable Bowel Syndrome is a functional gastrointestinal disorder that has been associated with alterations in the gut microbiome. Some studies have reported a decrease in microbial diversity and an increase in the ratio of Firmicutes to Bacteroidetes in IBS patients. Dietary triggers, such as FODMAPs (fermentable oligosaccharides, disaccharides, monosaccharides, and polyols) and gluten, have been identified as potential contributors to IBS symptoms in some individuals. Genetic factors may also play a role in IBS susceptibility, with several candidate genes involved in serotonin signaling, immune regulation, and epithelial barrier function.
7.3.2. Potential impact of SBM/PIS on IBS management and treatment
The SBM/PIS could aid in the management of IBS by identifying individual-specific microbiome patterns and dietary triggers associated with symptoms. The AI-driven system could develop personalized dietary recommendations and targeted probiotic therapy to alleviate symptoms and promote a healthy gut microbiome. By continuously monitoring the gut microbiome and adapting interventions based on patient response, the SBM/PIS could potentially provide long-term symptom relief and improve quality of life for IBS patients. While a complete “cure” for IBS may not be possible due to the multifactorial nature of the disorder, the SBM/PIS could significantly reduce the burden of symptoms and help patients maintain a healthy gut environment.
7.4. Colorectal Cancer
7.4.1. Known links to gut microbiome, diet, and genetic/epigenetic profile
Colorectal cancer has been linked to alterations in the gut microbiome, with studies showing an enrichment of certain bacterial species, such as Fusobacterium nucleatum and Escherichia coli, in colorectal tumors. A diet high in red and processed meats, as well as low in fiber, has been associated with an increased risk of colorectal cancer. Genetic factors, such as mutations in the APC, KRAS, and TP53 genes, play a significant role in colorectal cancer development, and epigenetic modifications, such as DNA methylation and histone modifications, have also been implicated in the disease.
7.4.2. Potential impact of SBM/PIS on colorectal cancer prevention and treatment
The SBM/PIS could potentially contribute to the prevention and treatment of colorectal cancer by maintaining a healthy gut microbiome and identifying early microbial signatures associated with precancerous lesions or early-stage tumors. The AI-driven system could develop targeted interventions, such as the use of synthetic immune cells or TNCOs, to eliminate harmful bacteria or modulate the immune response to prevent tumor growth. By continuously monitoring the gut microbiome and adapting interventions based on individual risk profiles, the SBM/PIS could help reduce the incidence of colorectal cancer and improve treatment outcomes. However, given the significant role of genetic and epigenetic factors in colorectal cancer development, the SBM/PIS would likely be most effective as part of a comprehensive prevention and treatment strategy that also includes regular screening, lifestyle modifications, and targeted therapies based on individual genetic profiles.
7.5. Obesity and Metabolic Disorders
7.5.1. Known links to gut microbiome, diet, and genetic/epigenetic profile
Obesity and related metabolic disorders, such as metabolic syndrome and non-alcoholic fatty liver disease (NAFLD), have been associated with alterations in the gut microbiome. Studies have shown that obese individuals often have a lower ratio of Bacteroidetes to Firmicutes compared to lean individuals, and this shift in microbial composition has been linked to increased energy harvest from the diet. High-fat, high-sugar diets have been identified as major contributors to obesity and metabolic disorders, and genetic factors, such as variations in the FTO, MC4R, and PPARG genes, have also been implicated in the development of these conditions.
7.5.2. Potential impact of SBM/PIS on obesity and metabolic disorder management
The SBM/PIS could play a significant role in the management of obesity and related metabolic disorders by modulating the gut microbiome to promote a healthier microbial composition and improve metabolic function. The AI-driven system could develop personalized dietary recommendations and targeted probiotic therapy to reduce energy harvest, improve insulin sensitivity, and alleviate inflammation. By continuously monitoring the gut microbiome and adapting interventions based on individual responses, the SBM/PIS could help individuals achieve and maintain a healthy weight, as well as improve overall metabolic health. While the SBM/PIS may not be a standalone “cure” for obesity and metabolic disorders, it could be a powerful tool in a comprehensive management strategy that also includes lifestyle modifications, such as regular exercise and a balanced diet, and medical interventions when necessary.
7.6. Type 2 Diabetes
7.6.1. Known links to gut microbiome, diet, and genetic/epigenetic profile
Type 2 diabetes has been linked to alterations in the gut microbiome, with studies showing a decrease in microbial diversity and an increase in opportunistic pathogens in diabetic individuals. A diet high in refined carbohydrates and low in fiber has been associated with an increased risk of type 2 diabetes, and genetic factors, such as variations in the TCF7L2, PPARG, and KCNJ11 genes, have also been implicated in the development of the disease. Epigenetic modifications, such as DNA methylation and histone modifications, have been shown to play a role in the regulation of glucose metabolism and insulin sensitivity.
7.6.2. Potential impact of SBM/PIS on type 2 diabetes prevention and management
The SBM/PIS could contribute to the prevention and management of type 2 diabetes by maintaining a healthy gut microbiome and improving glucose metabolism. The AI-driven system could develop personalized dietary recommendations and targeted probiotic therapy to promote the growth of beneficial bacteria, such as Akkermansia muciniphila, which has been shown to improve insulin sensitivity and reduce inflammation. By continuously monitoring the gut microbiome and adapting interventions based on individual responses, the SBM/PIS could help individuals maintain optimal blood sugar control and reduce the risk of diabetes-related complications. While the SBM/PIS may not be a standalone “cure” for type 2 diabetes, it could be a valuable tool in a comprehensive management strategy that also includes lifestyle modifications, such as regular exercise and a balanced diet, and medical interventions, such as insulin therapy or oral hypoglycemic agents, when necessary.
7.7. Autoimmune Diseases (e.g., rheumatoid arthritis, multiple sclerosis)
7.7.1. Known links to gut microbiome, diet, and genetic/epigenetic profile
Autoimmune diseases, such as rheumatoid arthritis and multiple sclerosis, have been linked to alterations in the gut microbiome, with studies showing a decrease in microbial diversity and an increase in potentially harmful bacteria in affected individuals. Dietary factors, such as a high-fat, high-sugar Western diet, have been associated with an increased risk of autoimmune diseases, and genetic susceptibility plays a significant role in the development of these conditions, with several identified risk alleles involved in immune regulation and tolerance.
7.7.2. Potential impact of SBM/PIS on autoimmune disease management and treatment
The SBM/PIS could potentially contribute to the management and treatment of autoimmune diseases by modulating the gut microbiome to promote immune homeostasis and reduce inflammation. The AI-driven system could develop personalized interventions, such as targeted probiotic therapy or the use of synthetic immune cells or TNCOs, to regulate the immune response and prevent or alleviate disease flare-ups. By continuously monitoring the gut microbiome and adapting interventions based on individual responses, the SBM/PIS could help individuals maintain a healthy immune balance and improve quality of life. However, given the complex nature of autoimmune diseases and the significant role of genetic factors in their development, the SBM/PIS would likely be most effective as part of a comprehensive management strategy that also includes immunomodulatory medications, lifestyle modifications, and targeted therapies based on individual genetic profiles.
7.8. Neurological Disorders (e.g., Parkinson’s disease, Alzheimer’s disease)
7.8.1. Known links to gut microbiome, diet, and genetic/epigenetic profile
Neurological disorders, such as Parkinson’s disease and Alzheimer’s disease, have been linked to alterations in the gut microbiome, with studies showing a decrease in microbial diversity and an increase in potentially harmful bacteria in affected individuals. Dietary factors, such as a high-fat, high-sugar Western diet, have been associated with an increased risk of neurological disorders, and genetic susceptibility plays a significant role in the development of these conditions, with several identified risk alleles involved in neurodegenerative processes and immune regulation.
7.8.2. Potential impact of SBM/PIS on neurological disorder prevention and management
The SBM/PIS could potentially contribute to the prevention and management of neurological disorders by maintaining a healthy gut microbiome and modulating the gut-brain axis. The AI-driven system could develop personalized interventions, such as targeted probiotic therapy or the use of synthetic immune cells or TNCOs, to reduce inflammation, protect neurons, and promote healthy brain function. By continuously monitoring the gut microbiome and adapting interventions based on individual responses, the SBM/PIS could help individuals maintain optimal cognitive function and potentially slow the progression of neurodegenerative disorders. However, given the complex nature of neurological disorders and the significant role of genetic and environmental factors in their development, the SBM/PIS would likely be most effective as part of a comprehensive prevention and management strategy that also includes lifestyle modifications, such as regular exercise and a balanced diet, and targeted therapies based on individual genetic profiles.
7.9. Allergies and Asthma
7.9.1. Known links to gut microbiome, diet, and genetic/epigenetic profile
Allergies and asthma have been linked to alterations in the gut microbiome, with studies showing a decrease in microbial diversity and an increase in potentially harmful bacteria in affected individuals. Dietary factors, such as a low-fiber, high-processed food diet, have been associated with an increased risk of allergies and asthma, and genetic susceptibility plays a significant role in the development of these conditions, with several identified risk alleles involved in immune regulation and barrier function.
7.9.2. Potential impact of SBM/PIS on allergy and asthma prevention and management
The SBM/PIS could potentially contribute to the prevention and management of allergies and asthma by maintaining a healthy gut microbiome and promoting immune tolerance. The AI-driven system could develop personalized interventions, such as targeted probiotic therapy or the use of synthetic immune cells or TNCOs, to regulate the immune response and prevent or alleviate allergic reactions and asthma symptoms. By continuously monitoring the gut microbiome and adapting interventions based on individual responses, the SBM/PIS could help individuals maintain a healthy immune balance and reduce the burden of allergies and asthma. However, given the complex nature of these conditions and the significant role of environmental factors, such as exposure to allergens and pollutants, in their development, the SBM/PIS would likely be most effective as part of a comprehensive prevention and management strategy that also includes lifestyle modifications, such as allergen avoidance and air quality control, and targeted therapies, such as immunotherapy or anti-inflammatory medications, when necessary.
7.10. Polycystic Ovary Syndrome (PCOS)
7.10.1. Known links to gut microbiome, diet, and genetic/epigenetic profile
Polycystic Ovary Syndrome (PCOS) is a complex endocrine disorder that has been associated with alterations in the gut microbiome. Studies have shown that women with PCOS often have a lower diversity of gut bacteria and an increased abundance of certain bacterial species, such as Bacteroides vulgatus and Escherichia coli. Additionally, PCOS has been linked to dietary factors, such as high consumption of refined carbohydrates and saturated fats, which can influence the gut microbiome composition. Genetic susceptibility also plays a role in PCOS, with several identified risk alleles involved in insulin resistance, androgen synthesis, and inflammation.
7.10.2. Potential impact of SBM/PIS on PCOS management and treatment
The SBM/PIS could potentially contribute to the management and treatment of PCOS by modulating the gut microbiome to improve insulin sensitivity, reduce inflammation, and regulate androgen production. The AI-driven system could develop personalized interventions, such as targeted probiotic therapy or dietary modifications, to promote the growth of beneficial bacteria and alleviate PCOS symptoms. By continuously monitoring the gut microbiome and adapting interventions based on individual responses, the SBM/PIS could help women with PCOS achieve better hormonal balance, improve fertility, and reduce the risk of associated metabolic complications, such as type 2 diabetes and cardiovascular disease. However, given the multifactorial nature of PCOS and the significant role of genetic and lifestyle factors in its development, the SBM/PIS would likely be most effective as part of a comprehensive management strategy that also includes lifestyle modifications, such as regular exercise and a balanced diet, and medical interventions, such as insulin-sensitizing agents or anti-androgenic medications, when necessary.
7.11. Conclusion
The gut microbiome plays a crucial role in the development and progression of various diseases, ranging from gastrointestinal disorders to neurological conditions. The Synthetic Biome Manager (SBM) and Parallel Immune System (PIS) offer a promising approach to addressing these gut microbiome-related diseases by continuously monitoring the gut microbiome, identifying dysbiosis patterns, and developing personalized interventions to restore balance and promote health.
While the extent to which the SBM/PIS can provide a “cure” or long-term management solution varies depending on the specific disease and individual factors, this innovative system has the potential to significantly improve patient outcomes and quality of life. By maintaining a healthy gut microbiome, identifying early disease signatures, and developing targeted interventions, the SBM/PIS could contribute to the prevention, management, and treatment of a wide range of gut microbiome-related diseases.
However, it is important to recognize that the gut microbiome is just one piece of the complex puzzle of disease development and progression. Genetic, epigenetic, environmental, and lifestyle factors also play significant roles in shaping health outcomes. As such, the SBM/PIS would likely be most effective as part of a comprehensive, personalized approach to disease prevention and management that takes into account these multiple factors and integrates various therapeutic strategies, such as lifestyle modifications, medical interventions, and targeted therapies based on individual genetic profiles.
As research continues to unravel the intricate connections between the gut microbiome and human health, the SBM/PIS represents a promising frontier in the development of personalized, precision medicine approaches to address the growing burden of gut microbiome-related diseases.