Electrical Impedance Tomography (EIT) is an emerging medical imaging technique that creates pictures of the inner structures of the body in a completely safe, non-invasive way. It works by gently applying small, imperceptible electrical currents on the skin using electrodes. As these currents pass through body tissues, they encounter different levels of impedance – resistance to electrical flow – which manifests as voltages measured again on the skin. Unlike X-rays or MRIs, EIT does not require potentially harmful ionizing radiation or magnets.
Since cancerous growths have different cell structures and water content compared to healthy tissues, they conduct electricity differently. By using algorithms to convert many skin voltage measurements around the body into an image, EIT can map these electrical property differences. This allows benign and malignant tumors – and even microcalcifications – to be distinguished clearly without recalls or biopsies.
EIT is still an early-stage technology, but its unique ability to harmlessly “see” tissue structure and composition shows enormous promise. Integrating it with phased array engineering now enables more advanced, higher resolution images able to change cancer diagnostics. The safe, comfortable and affordable EIT examination may one day become a routine part of healthcare.
Limitations of Current Diagnostic Tools
The most common breast cancer diagnostic tools face considerable limitations. Mammograms use harmful ionizing radiation and painful compression. Their resolution is insufficient to catch early tumors, frequently generating false positives that lead to stressful and unnecessary follow-up tests and biopsies. Ultrasounds rely heavily on operator skill and struggle to penetrate dense breast tissue. Dynamic contrast MRIs require the injection of contrast dye agents which are expensive and can cause allergic reactions or kidney damage. These tools also involve long scan times and accessibility issues for many patients. Unlike these imaging modalities, phased array EIT offers high resolution 3D maps of breast tissue in a comfortable, non-toxic way using only safe levels of electrical current. The sensitivity of impedance mapping may allow for diagnoses without recalls or biopsies. As an affordable technology that requires no chemicals or radiation, phased array EIT has the potential to complement and enhance the entire pipeline of breast cancer detection for all patients.
Reimagining the Future of Breast Cancer Diagnosis:
The Promise of Phased Array EIT In an era when one in eight women will develop breast cancer in their lifetime, early and accurate detection remains impeded by suboptimal diagnostic tools that expose patients to harm while still struggling to discern tumors at the most treatable stages. However, a new approach promises to revolutionize how we image, screen and ultimately save the lives of those at risk of cancer. By integrating phased array technology with Electrical Impedance Tomography (EIT), a non-invasive current-imaging technique, researchers have paved an avenue to dramatically enhance EIT’s resolution and utility in mapping the subtle electrical signatures of malignant tissues—all while avoiding the downsides of existing cancer diagnostic pipelines.
How Phased Array EIT Achieves a New Level of Clarity
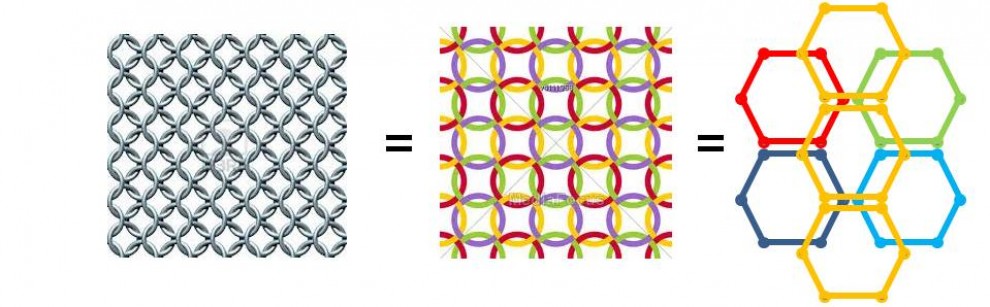
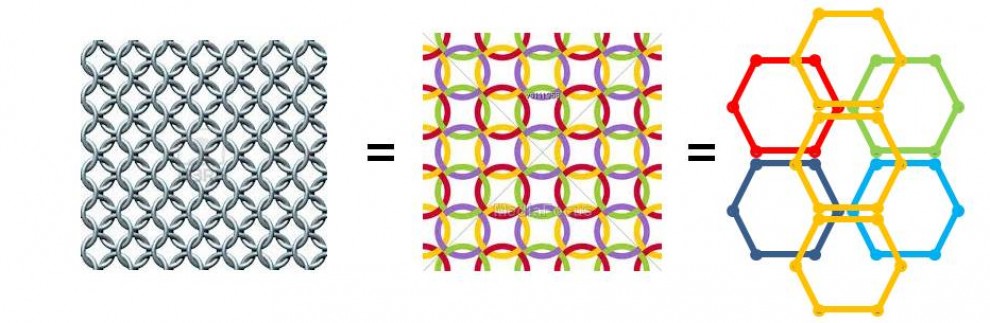
Phased array EIT centers around the use of a configurable grid of transmitter and receiver electrodes that steer localized clusters of current pulses dynamically in and around target tissues. By subtly manipulating the shape, directionality and synchronization of these clusters, the system generates fine-grained three-dimensional impedance maps with previously unattainable detail down to the level of microcalcifications and tumor angiogenesis. At the same time, advanced computational algorithms reconstruct artefact-free images from multifaceted data gathered through the technique’s elegant and intricate current steering approach.
Phased array EIT improves resolution through the use of multiple transmitting and receiving electrodes that can manipulate the shape, timing, and directionality of electrical current pulses. By subtly and rapidly altering the phase relationships between electrodes, the resulting constructive and destructive interference patterns can be used to focus current into tighter beams that scan across smaller regions of tissue. This allows more discrete sampling and mapping of impedance properties. Advanced algorithms can then reconstruct high-resolution images reflecting anomalies. Compared to conventional EIT with fixed electrode configurations and diffuse current patterns, phased array EIT enables superior focusing and targeting of cancerous tissues while also gathering robust data through its dynamic pulses. With hundreds of sensing elements that can pulse in intricate patterns, detailed 3D maps of the electrical properties of breast tissue can be built to reveal tumors or microcalcifications invisible to other modalities.
When integrated into a practical, patient-comfortable examination device, phased array EIT promises detection specificity and sensitivity well beyond seen in error-prone mammograms, operator-dependent ultrasounds, and toxic contrast MRIs. The affordability and safety profile empowers patients to monitor their breast health more frequently and catch the subtle changes that so often escalate into late stage disease with current modalities handicapped by their cost and access barriers. With further research and innovation, guided electrical scanning via phased arrays could salvage and transform the difficult diagnostic odyssey millions embark on each year.
Realizing the Potential Through Collaboration
Still, harnessing the full capability of phased array EIT requires breaking down knowledge silos and embracing multidisciplinary perspectives. Engineers, computational experts, clinicians and public health leaders must bridge their efforts to assess needs, prototype designs and analyze clinical outcomes. Funding and partnerships between academics, non-profits and industry can accelerate this effort. And active engagement with patients is critical for addressing real-world diagnostic challenges in an ethical, sensitive way. By recognizing each stakeholder’s unique yet unified role in this endeavor, a technology once restricted to radar systems could soon guide breast cancer care into an era where saving lives is no longer impeded by the tools meant to safeguard them.